
Happy New Year!
Congratulations on surviving a busy, dynamic and chaotic 2024 in healthcare. They say there is order in chaos. I believe this to be true, but still looking for it. I recently came across an excerpt from a book that resonated. Thought you might find it valuable on your journey.
To thrive in ambiguity means to be open to more than one interpretation of what you’re experiencing. It’s not about having “the solution” or even the destination in mind. It’s about having confidence in the journey.
These are good words of advice in times like this. I have tremendous confidence in the journey. I am equally confident we can harness the power of data innovation, analytics, and AI to drive positive, lasting impact along the way. The important thing is to take a step into the chaos, learn from the experience, course-correct as needed, believe you will eventually arrive at your destination, and enjoy the journey along the way.
In future blogs this year, we will focus on how the analytics and AI community is navigating the care ecosystem in 2025: what’s working and not working. To frame these blogs, let’s take a look at 2024 and a few trends that will shape 2025. Let’s get started.
2024 Year in Review
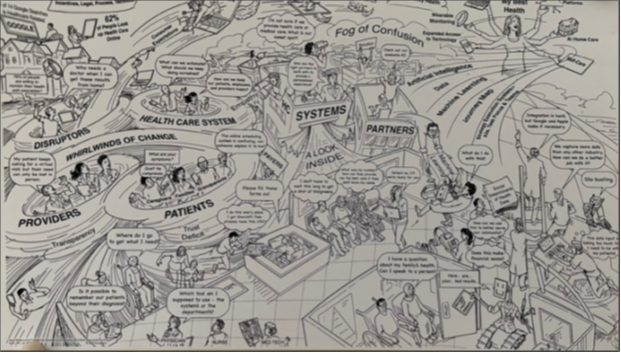
Let’s take a look at the care ecosystem as we enter the New Year. Below is an illustration I came across several years ago that has aged well in describing the complexities and level of change we are experiencing in the care ecosystem – opportunities and change galore.
Let’s dive deeper into 2024 trends that will continue to shape this care ecosystem in 2025.
Mergers & Acquisitions Continue Unabated: Hospital acquisitions continue somewhat quietly throughout the year. Per Cain Brothers, by the end of the third quarter, 57 hospital mergers and acquisitions were announced, nearly surpassing the 59 deals recorded in 2022 and on track to match or exceed the 75 deals in 2023. Quest and LabCorp continued their journey to absorb hospital labs (nearly a dozen), and private equity continues to consolidate dentistry and GI practices, and expand ambulatory surgical centers. This trend will only continue or accelerate in 2025.
Financial Stability Remains Uneven: 2024 is shaping up to be an improvement over 2023. The Kaufman Hall Year-To-Date Operating Margin Index for October 2024 was 4.4%. A year ago, it was 2.3%. This is good news. According to the chief healthcare executive, the bad news is that “the top third of hospitals and health systems are experiencing very large improvements. But roughly two-thirds of the nation’s hospitals are improving slightly or stagnating. As many as 40% of hospitals are losing money in 2024, according to Kaufman Hall.” This means many healthcare systems are at risk of closing down or being consolidated if they don’t improve their situation.
Care Deserts Expand: More than 30% of rural hospitals are at risk of closure, per the Center for Healthcare Quality and Payment Reform Report. These closures would impact hundreds of thousands of people who need critical care to manage cardiovascular and maternity health.
Ransomware Threats Escalate: Ransomware attacks grew significantly in 2024. According to Sophos, 67% of healthcare systems were hit by ransomware attacks, up from 60% in 2023.
Physicians Moving from Independent Practice: According to the Physicians Advocacy Institute (PAI) reports, nearly 78% of physicians are employed by hospitals or corporate entities, up from 62% in 2019.
Health and Human Services Shakeup: The new presidential administration promises significant changes in health and human services, including cost-cutting, layoffs, restructuring, policy and regulatory changes, and so on. At a minimum, this will impact CMS, FDA and NIH, and will have a ripple effect across the entire care ecosystem.
Retail Health Landscape Shifting: As nascent and smaller care providers continue to grow their patient population, several larger, prominent players are rethinking their strategy. Walmart exited healthcare, while Humana is going deeper by leasing clinical space from Walmart. Walgreens and CVS are struggling and likely to narrow their scope, and Amazon One Medical is expanding. None have yet figured out how to integrate with existing provider organizations as a referral source effectively.
Value-Based Care Growth Continues: Value-based care (VBC) continues to grow steadily. According to the Centers for Medicare & Medicaid Services, VBC models have seen a 25% increase in healthcare provider participation from 2023 to 2024. This growth continued in 2024, with Medicare Advantage plans as a prominent example. In 2024, 32.8 million people were enrolled in Medicare Advantage plans, representing 54% of the eligible Medicare population. Though there have been issues, expect these issues to be sorted out as growth continues.
Managed Services Ramps Up: The adoption of traditional managed services like IT help desk, and application administration and support continues growing. In addition, organizations are looking to develop deeper relationships with vendor partners by expanding their support beyond traditional IT services to include supply chain, revenue cycle, and enterprise analytics.
Responsible AI Gains Momentum: There is a critical need to establish a responsible AI framework for healthcare. To this end, many frameworks have been introduced over the past year: CHAI, CoDEx, HealthAI, TRAIN, WHO, NIST, ISO, and HAIP—and this is the short list. Over the next year, we must decide where and how to leverage these frameworks. Undoubtedly, there will be some consolidation and pruning as we work toward a more simplified framework.
Care Delivery Evolves: Care delivery continues shifting toward hybrid models that combine in-person, virtual, and automated care. Remote patient monitoring adoption grew in 2024. Hospital-at-home programs doubled to over 300 sites nationwide.
Digital front-door investments accelerated as health systems prioritize patient access and engagement. A majority of systems now offer self-scheduling, while AI-powered symptom checkers and triage tools saw growth in adoption.
Workforce optimization emerged as critical, with many health systems implementing AI-assisted documentation and staff scheduling. Virtual nursing programs expanded to address staffing gaps, growing from 100 to 250 programs nationwide.
Mental health integration into primary care settings increased, driven by rising demand and provider shortages. This includes both embedded behavioral health specialists and virtual collaborative care models.
Specialty care transformation gained momentum through hub-and-spoke models connecting academic medical centers with community providers. These partnerships grew in 2024, improving access to complex care while maintaining patients in local settings.
This is not a comprehensive list of trends. Other notable trends that took shape in 2024, and will further evolve in 2025, include provider and price transparency, research advancements, data interoperability, learning health systems, intelligent automation, AI agents, IoT, and command-line dashboards. However, this list gives a sense of the many forces for change in 2024 and foreshadows things to come in 2025.
Organizations that can effectively leverage data innovation, analytics, and AI will shape these trends and care ecosystem while others struggle to survive. Now, let’s look at a few trends that will likely shape the care ecosystem in 2025. Though I believe all these trends will play out, I’ve ordered most to least likely to happen in 2025.
1. Data Foundation Is King (Again)
Capitalizing on the trends below requires a trusted, scalable data foundation. Unfortunately, many organizations lack this essential component, hindering their ability to effectively leverage emerging analytics and artificial intelligence trends. Addressing this foundational gap is a critical step that must precede any attempt to capitalize on the trends below.
For many organizations, their data foundation resembles a patchwork of disparate solutions. These solutions have been cobbled together over time to address specific departmental needs without a cohesive, long-term strategy for reuse, maintainability or quality. As a result, organizations struggle with the absence of a single source of truth or a robust governance framework. This impedes their ability to safely, efficiently, and effectively advance their analytics and AI journey.
To overcome these challenges, organizations must develop a unified data foundation. This involves establishing standardized data pipelines, implementing data governance policies, and ensuring the quality and reliability of data across all departments. Modern data platforms with integrated governance tools can help organizations create a trusted environment for data sharing, analytics and AI.
A scalable data foundation is also critical for handling exponential data volumes, complexity and growth. This is where the cloud plays a transformative role. By migrating to the cloud, organizations can access unlimited storage and processing capabilities, enabling them to handle vast amounts of structured and unstructured data. This is particularly important for generative AI applications, which require significant computational resources to process and analyze data efficiently.
Cloud also offers a way to reduce ongoing infrastructure and administration costs substantially. To realize these gains, organizations must develop effective FinOps capabilities.
Fortunately, many organizations realize the need to shore up their foundations to effectively leverage analytics and AI to drive meaningful value and impact. To continue their data innovation journey without stopping, leading organizations are adopting a federated, agile approach that allows them to build out this foundation while demonstrating value incrementally and often. We will discuss this further in the next section.
2. Federated Operating Models Gain Traction
Legacy centralized, transactional approaches to analytics and AI delivery that are rigid, top-down, and project-oriented are giving way to a federated and collaborative model. The legacy approach is designed for a more static environment and struggles to adapt to today's dynamic and chaotic care ecosystem.
By contrast, the federated, collaborative model empowers decentralized teams to make agile, real-time decisions. This shift is a response to technological advancements and a cultural transformation, emphasizing trust, autonomy and cross-functional collaboration.
Adopting a bottom-up decision-making structure aligns analytics and AI initiatives more closely with the immediate needs of care providers and patients. It also allows for more customized and context-aware systems that address specific challenges in different departments or units.
This approach facilitates faster delivery of data products, minimizes bureaucratic delays, and fosters innovation by encouraging structured experimentation at all organizational levels.
From an operational perspective, federated models can lead to significant productivity gains.
Employees empowered to make decisions and contribute meaningfully to initiatives are likelier to be engaged and satisfied in their roles. This enriched work environment boosts morale and helps attract and retain top talent in an increasingly competitive industry.
This model is not without challenges. Organizations must invest in robust, flexible data governance frameworks to ensure consistency, security and compliance across decentralized teams. Additionally, fostering a culture of collaboration and continuous learning is essential to realize the full potential of this approach.
That said, those who can overcome these challenges will thrive, while those who don't will struggle to keep up. We have covered this topic extensively in this blog. For a primer, see the first three pieces in this series: Accelerating Your Data Innovation Journey in the Healthcare Industry, Operating Like a Startup, and Think Like an Entrepreneur.
3. Balancing Cost Reduction and Growth
With the growth in competition driven by new players and mergers and acquisitions, there will be significant pressure to harness analytics and AI to reduce costs and improve profitability by reducing waste and redundancy in the system.
Leading organizations will balance this ruthless focus on cost reduction by leveraging analytics and AI to promote growth and greater profitability, improving outcomes and enriching the patient and provider experience.
Analytics and AI are not only tools for cutting costs—they are powerful drivers of growth that contribute to profitability. A prime example is AI-enabled personalized medicine. By analyzing vast amounts of patient data, AI can help tailor treatment plans to individual patients, leading to better clinical outcomes and increased patient satisfaction.
Let’s take a closer look. Healthcare organizations that use AI to optimize cancer treatment pathways can enhance patient recovery rates while strengthening their reputation as leaders in advanced care. Similarly, predictive modeling in revenue cycle management allows organizations to identify financial bottlenecks and improve revenue collection, creating new growth opportunities.
Balancing cost reduction with investments in growth initiatives is critical for sustainable success. Leading organizations achieve this balance by reinvesting the savings from efficiency gains into innovative projects that enhance their strategic positioning. These organizations leverage analytics to streamline operations while simultaneously investing in cutting-edge research and patient-centered care initiatives. This dual focus has driven operational efficiency and improved patient experiences, enabling the organization to achieve sustainable growth and profitability.
Digital twins, for instance, enable healthcare organizations to simulate and optimize hospital operations, predict patient flow, and test new care delivery models in a virtual environment. However, perhaps the most transformative focus area will be achieving true interoperability— seamlessly connecting disparate data sources across the healthcare ecosystem. This will allow organizations to generate holistic, actionable insights, ultimately improving care coordination, reducing costs and driving better patient outcomes.
Healthcare organizations that successfully balance efficiency-driven cost reductions with growth-oriented innovation will emerge as leaders. By strategically leveraging analytics and AI, they will improve their financial health and create a more patient-centered and provider-friendly healthcare ecosystem.
4. GenAI Delivers Tangible Value
GenAI proof-of-concepts and pilot programs will start to demonstrate positive impact and value for healthcare organizations as they explore where and how to defer new or sunset existing product investments by doing it themselves.
Areas such as diagnostics, patient flow optimization, patient engagement, and administrative tasks like billing and supply chain will benefit the most from GenAI due to its ability to analyze structured and unstructured data to generate predictive and prescriptive insights—shifting operations from reactive to proactive.
These early successes will drive organizations to rethink traditional approaches to technology investment, allowing them to defer new product acquisitions and phase out legacy systems instead of building customized systems in-house. These organizations will seek experienced vendor partners to help them on this journey.
This adoption of GenAI will not be without its challenges. Healthcare organizations will face hurdles like data privacy and ethics concerns, regulatory compliance, integration with existing systems, and the need for workforce and patient education.
Addressing these challenges will require robust, scalable data governance policies, investments in cybersecurity measures, strategic planning for technology integration, and comprehensive training programs to adapt to new tools and workflows.
Health systems will unlock unprecedented gains by harnessing these advanced capabilities. For example, automated coding can significantly reduce errors and processing times in claims management, leading to faster reimbursements and lower administrative costs.
Census prediction enables better resource allocation and staffing decisions, improving operational efficiency and patient care delivery. As efficiency improves, patients will experience reduced costs, shorter wait times, and higher-quality care due to more effective use of resources and personnel.
Clinical monitoring continuously analyzes patient vitals, lab values, medication responses and clinical notes to predict adverse events before they occur. This early warning system allows care teams to intervene proactively, improving patient outcomes, and reducing ICU transfers and hospital length of stay. Other clinical opportunities will be improving medication safety, reducing patient infections, and improving the speed and quality of diagnosis (imaging and lab), and improved outcomes resulting from fine-grain phenotyping to tailor treatments.
However, this transition raises security concerns regarding data breaches and compliance with healthcare regulations like HIPAA. Organizations will also need to learn how to leverage the vast tools available to innovate with data and excel in fin-ops to do this cost-effectively.
Final Thoughts
The healthcare ecosystem in 2025 will continue to be shaped by the interplay of patient demands, clinical needs, research integration, evolving care models, competitive landscape, regulation and policy, and technology. Organizations that prioritize foundational improvements, adopt flexible operating models, and leverage analytics and AI to balance efficiency with growth will emerge as leaders in this dynamic landscape.
As we embark on this journey together in 2025, I look forward to sharing insights, success stories, and actionable strategies to help accelerate your data innovation journey. Let’s thrive in the ambiguity and build a future-ready healthcare ecosystem—one step at a time.
Happy New Year and here’s to an exciting journey in 2025! Please let me know if you have an ideas and would like to contribute to the series.